Introduction to Headache Medicine

If you suffer from migraine headaches there might be a chance that some of your pain is referred from your neck. 64% of patients seen by doctors report neck pain as a component of their migraine.
Cervicogenic Headache or CGHA, refers to head pain that is generated by, or referred by, cervical structures such as bone, joint, disc, and/or soft tissue (muscles, ligaments, etc). Precipitating factors include traumatic injury, secondary processes such as osteoarthritis, or genetic predispositions such as spondylolisthesis.
These “neck disorders” may also “trigger” primary headache syndromes, such as migraine, tension-type headache, or hemicrania continua.
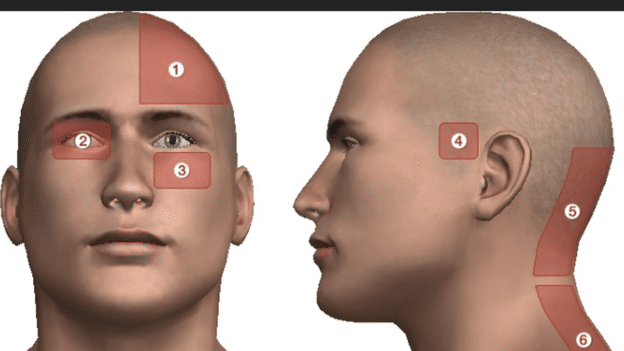
Patients with CGHA have neck pain that is usually described as constant, dull, non-throbbing pain. The headache is one-sided and at the back of the head. You can also have pain around the eye (periorbitally) or at the side, top or front of the head.
CGHA share similar symptoms with migraine such as nausea, emesis, photo and phonophobia, worsening pain with activity, even a throbbing sensation, and pain in the arm or shoulder!
Is Migraine Medicine a specialty?
More than 50% of individuals experiencing headache have only been treated symptomatically, with no appropriate diagnosis established. Most patients with headache are *not* being treated by specialists in Headache Medicine because of the small number of specialists.
Advanced technology and clinical innovation offers more treatment options than ever before. However, these diseases are still largely misunderstood.
Finding the right treatment options for you requires nuanced and adaptable insight. Differentiating migraines from other headache disorders means faster relief through more targeted treatments based on the type of headache and puts you more in control of your pain.
Oswego Physical Therapy Clinic is partnering with *Ropana Migraine Health* to offer you alternative treatments for your migraine headaches. Neurologists Dr. Delman and Dr. Gurjeet Singh are *Board-Certified Neurologists *with additional *Board Certification in Headaches* who offer comprehensive and holistic management of headaches.
What to do with that 800 lbs Gorilla in your head? (Perhaps it feels like a screaming Tiger).
Cervicogenic headaches and tension headaches are conditions, among others, which are treatable in Physical Therapy. Recently a client reported having cluster headaches. His pain was intermittent and shot through to his right eye and temple.
The possible sources and intricacies of cervicogenic headaches are endless and can be related to poor posture, too much stretching, not enough strengthening or vice versa, lack of circulation in postural muscles, weakness, arthritis, etc.
He felt that his pain was migrainous but we also learned that it was coming from his neck! It is not unusual for someone to know whether they are having a migraine, a cluster headache, or a tension-headache.
Chronic migraines can be *“mixed” or “combination”, for example, it can have *features of migraine and cervicogenic headache*.
His upper cervical spine had signs of instability, better termed hypermobility. In addition, his upper cervical spine was sending referred pain into the head (upper cervical radicular pain). He tested positive for provocation tests. He also had *suboccipital* muscle restrictions at the base of his skull causing pain and tightness sensation there. Based on the findings of a PT evaluation the idea is to relieve the stresses and strains on pain provoking structures of the neck, relieve tension, restore mobility, or treat hypermobile neck issues with stabilization exercises.
Sometimes the C1 vertebrae is shifted or there are facet (joint) issues. Providing manual therapy with massage to relax muscles, friction on trigger-points, mobilizing joints in the neck, avoiding certain stretching exercises, and emphasizing strengthening of muscles at the upper back and neck can be very effective.

Other treatment ideas:
Peppermint oil. This comes in a variety of forms such as incense sticks, tea, and oil. The oil may help control blood flow in the body and open up the sinuses for better oxygen flow.
1. The importance of sleep: Lack of sleep can trigger migraine attacks. People who experience migraine attacks often report sleep as an effective therapy for migraine. During the sleep the glymphatic system washes away toxic waste products accumulated in the brain (amyloid proteins) that build up when awake. It is possible that getting enough level 4 non-REM sleep is restorative in reducing migraines. The first 4 hours of your sleep cycle is predominantly Non-REM, the last 4 hours are REM. Getting enough of both is extremely important. Thomas Walker in his book “Why we Sleep” recommends 8 hours of sleep per night.
2. Keep a headache diary. *Keeping detailed records of headache episodes can help provide additional insight about triggers and how to avoid them. Write down what you were doing, what foods you ate, what medications you took prior to your migraine attack, etc. This helps to identify your triggers.
3. Magic Gel Migraine Ice Head Wrap Headache Cap. *This is a hoody with built in ice packs.
Conclusion
All migraines are headaches, but not all headaches are migraines. Learn as much as you can from a variety of sources and find out what works. Find a clinician who can provide you with a diagnosis (source of the problem) and who can offer you tools to address your issues.
The more I learn about headaches the more I appreciate its complexity. No two people ever present with the same two headaches. Treating your neck pain may be an adjunct to being able to manage your migraine headaches!
I would love to hear from you about your headache condition. Do not hesitate to contact me if you would like to discuss possible treatment options.
Source: “Headache and Migraine Biology” Dr. Seymour Diamond.

